Autism is running prevalent today. My question was, is it getting worse or is it easier to detect due to new brain spects and other technology. I think it is a little of both. I enjoyed learning the facts below. I have great appreciation for all of you parenting and working with these precious children. Enjoy the following from the Autism Society. ~Sandy
What is Autism:
Autism spectrum disorder (ASD) is a complex developmental disability; signs typically appear during early childhood and affect a person’s ability to communicate, and interact with others. ASD is defined by a certain set of behaviors and is a “spectrum condition” that affects individuals differently and to varying degrees. There is no known single cause of autism, but increased awareness and early diagnosis/intervention and access to appropriate services/supports lead to significantly improved outcomes. Some of the behaviors associated with autism include delayed learning of language; difficulty making eye contact or holding a conversation; difficulty with executive functioning, which relates to reasoning and planning; narrow, intense interests; poor motor skills’ and sensory sensitivities. Again, a person on the spectrum might follow many of these behaviors or just a few, or many others besides. The diagnosis of autism spectrum disorder is applied based on analysis of all behaviors and their severity.
In 2016, the Centers for Disease Control and Prevention issued their ADDM autism prevalence report. The report concluded that the prevalence of autism had risen to 1 in every 68 births in the United States – nearly twice as great as the 2004 rate of 1 in 125 – and almost 1 in 54 boys. The spotlight shining on autism as a result has opened opportunities for the nation to consider how to serve families facing a lifetime of supports for their children. In June 2014, researchers estimated the lifetime cost of caring for a child with autism is as great as $2.4 million. The Autism Society estimates that the United States is facing almost $90 billion annually in costs for autism. (This figure includes research, insurance costs and non-covered expenses, Medicaid waivers for autism, educational spending, housing, transportation, employment, related therapeutic services and caregiver costs.)
Know the signs: Early identification can change lives
Autism is treatable. Children do not “outgrow” autism, but studies show that early diagnosis and intervention lead to significantly improved outcomes. For more information on developmental milestones, visit the CDC’s “Know the Signs. Act Early” site.
HERE ARE SOME SIGNS TO LOOK FOR IN THE CHILDREN IN YOUR LIFE:
- Lack of or delay in spoken language
- Repetitive use of language and/or motor mannerisms (e.g., hand-flapping, twirling objects)
- Little or no eye contact
- Lack of interest in peer relationships
- Lack of spontaneous or make-believe play
- Persistent fixation on parts of objects
SYMPTOMS:
The characteristic behaviors of autism spectrum disorder may be apparent in infancy (18 to 24 months), but they usually become clearer during early childhood (24 months to 6 years).
As part of a well-baby or well-child visit, your child’s doctor should perform a “developmental screening,” asking specific questions about your baby’s progress. The National Institute of Child Health and Human Development (NICHD) lists five behaviors that warrant further evaluation:
- Does not babble or coo by 12 months
- Does not gesture (point, wave, grasp) by 12 months
- Does not say single words by 16 months
- Does not say two-word phrases on his or her own by 24 months
- Has any loss of any language or social skill at any age
Any of these five “red flags” does not mean your child has autism. But because the disorder’s symptoms vary so widely, a child showing these behaviors should be evaluated by a multidisciplinary team. This team might include a neurologist, psychologist, developmental pediatrician, speech/language therapist, learning consultant or other professionals who are knowledgeable about autism.
For more information, visit the Infants and Toddlers page or the CDC’s “Learn the Signs. Act Early” program.
DIAGNOSIS:
When parents or support providers become concerned that their child is not following a typical developmental course, they turn to experts, including psychologists, educators and medical professionals, for a diagnosis.
At first glance, some people with autism may appear to have an intellectual disability, sensory processing issues, or problems with hearing or vision. To complicate matters further, these conditions can co-occur with autism. However, it is important to distinguish autism from other conditions, as an accurate and early autism diagnosis can provide the basis for an appropriate educational and treatment program.
Other medical conditions or syndromes, such as sensory processing disorder, can present symptoms that are confusingly similar to autism’s. This is known as differential diagnosis.
There are many differences between a medical diagnosis and an educational determination, or school evaluation, of a disability. A medical diagnosis is made by a physician based on an assessment of symptoms and diagnostic tests. A medical diagnosis of autism spectrum disorder, for instance, is most frequently made by a physician according to the Diagnostic and Statistical Manual (DSM-5, released 2013) of the American Psychological Association. This manual guides physicians in diagnosing autism spectrum disorder according to a specific number of symptoms.
A brief observation in a single setting cannot present a true picture of someone’s abilities and behaviors. The person’s developmental history and input from parents, caregivers and/or teachers are important components of an accurate diagnosis.
An educational determination is made by a multidisciplinary evaluation team of various school professionals. The evaluation results are reviewed by a team of qualified professionals and the parents to determine whether a student qualifies for special education and related services under the Individuals with Disabilities Education Act (IDEA) (Hawkins, 2009).
CAUSES:
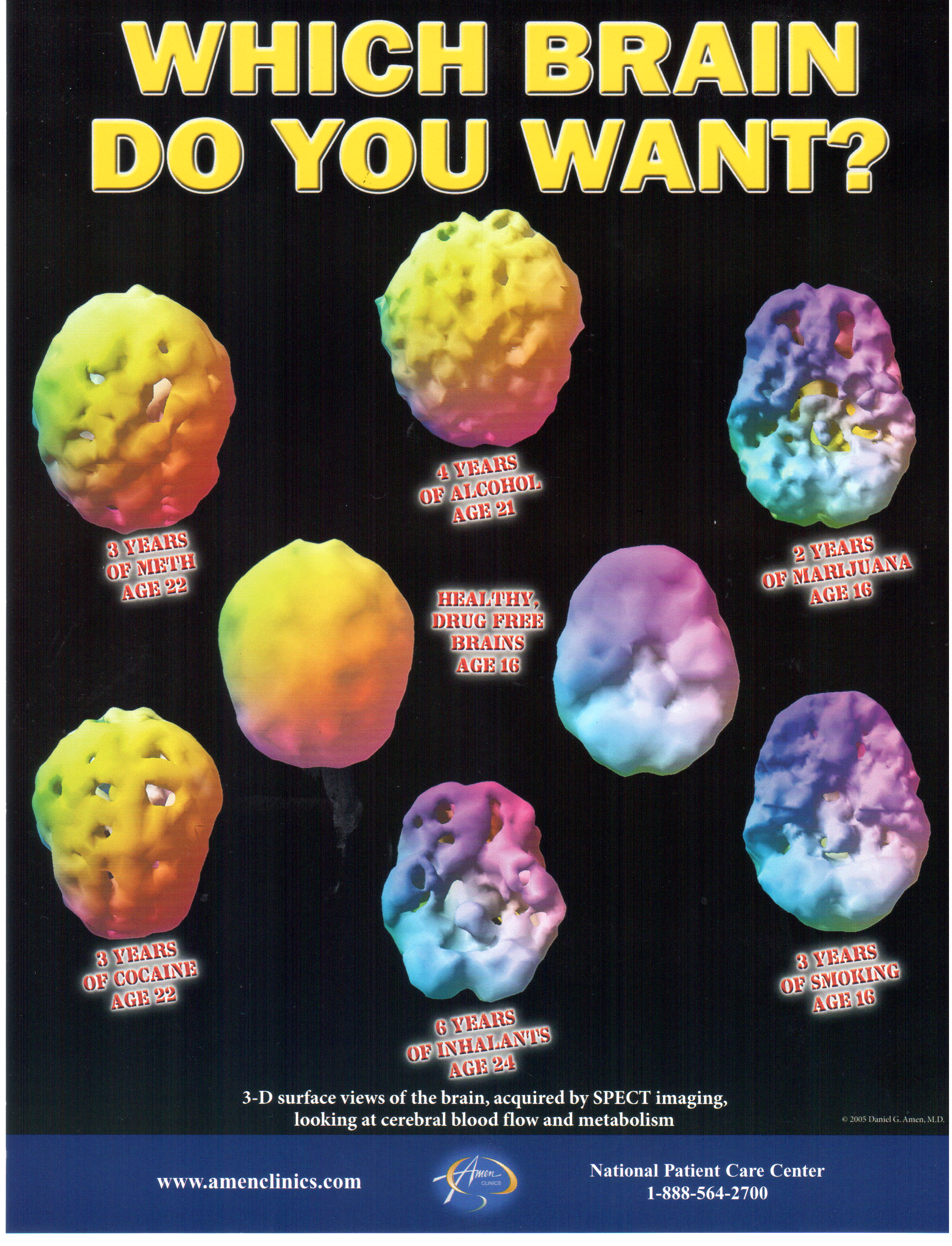
There is no known single cause for autism spectrum disorder, but it is generally accepted that it is caused by abnormalities in brain structure or function. Brain scans show differences in the shape and structure of the brain in children with autism compared to in neurotypical children. Researchers do not know the exact cause of autism but are investigating a number of theories, including the links among heredity, genetics and medical problems.
In many families, there appears to be a pattern of autism or related disabilities, further supporting the theory that the disorder has a genetic basis. While no one gene has been identified as causing autism, researchers are searching for irregular segments of genetic code that children with autism may have inherited. It also appears that some children are born with a susceptibility to autism, but researchers have not yet identified a single “trigger” that causes autism to develop.
Other researchers are investigating the possibility that under certain conditions, a cluster of unstable genes may interfere with brain development, resulting in autism. Still other researchers are investigating problems during pregnancy or delivery as well as environmental factors such as viral infections, metabolic imbalances and exposure to chemicals.
Genetic Vulnerability
Autism tends to occur more frequently than expected among individuals who have certain medical conditions, including fragile X syndrome, tuberous sclerosis, congenital rubella syndrome and untreated phenylketonuria (PKU). Some harmful substances ingested during pregnancy also have been associated with an increased risk of autism.
FACTS AND STATISTICS:
About 1 percent of the world population has autism spectrum disorder. (CDC, 2014)
Prevalence in the United States is estimated at 1 in 68 births. (CDC, 2014)
More than 3.5 million Americans live with an autism spectrum disorder. (Buescher et al., 2014)
Prevalence of autism in U.S. children increased by 119.4 percent from 2000 (1 in 150) to 2010 (1 in 68). (CDC, 2014) Autism is the fastest-growing developmental disability. (CDC, 2008)
Prevalence has increased by 6-15 percent each year from 2002 to 2010. (Based on biennial numbers from the CDC)
Autism services cost U.S. citizens $236-262 billion annually. (Buescher et al., 2014)
A majority of costs in the U.S. are in adult services – $175-196 billion, compared to $61-66 billion for children. (Buescher et al., 2014)
Cost of lifelong care can be reduced by 2/3 with early diagnosis and intervention. (Autism. 2007 Sep;11(5):453-63; The economic consequences of autistic spectrum disorder among children in a Swedish municipality. Järbrink K1.)
1 percent of the adult population of the United Kingdom has autism spectrum disorder. (Brugha T.S. et al., 2011)
The U.S. cost of autism over the lifespan is about $2.4 million for a person with an intellectual disability, or $1.4 million for a person without intellectual disability. (Buescher et al., 2014)
35 percent of young adults (ages 19-23) with autism have not had a job or received postgraduate education after leaving high school. (Shattuck et al., 2012)
It costs more than $8,600 extra per year to educate a student with autism. (Lavelle et al., 2014) (The average cost of educating a student is about $12,000 – NCES, 2014)
In June 2014, only 19.3 percent of people with disabilities in the U.S. were participating in the labor force – working or seeking work. Of those, 12.9 percent were unemployed, meaning only 16.8 percent of the population with disabilities was employed. (By contrast, 69.3 percent of people without disabilities were in the labor force, and 65 percent of the population without disabilities was employed.) (Bureau of Labor Statistics, 2014)
FOR MORE INFORMATION OR TO DONATE: https://www.autism-society.org/